Occupational Therapy with Integrative Health for Bipolar and Anxiety Disorders: Case Report – Now in Remission
By Emmy Vadnais, OTR/L and Carisa Hillman, OTS
This case report was created by Emmy Vadnais, OTR/L and fieldwork student, Carisa Hillman, OTS, while providing occupational therapy with integrative health for their client “Mary” in 2016. It was submitted to an OT and mental health journal, and after two years of revisions, including thorough assistance from an OT professor, it was not accepted. We were not told clearly how we could improve it for acceptance. We chose to not submit it to any other journals as we believe it will likely get more exposure and readership here. During this time Mary’s Bipolar Disorder diagnosis was reported to be in remission with a primary diagnosis of an Anxiety Disorder that she was managing well. Special thank you to Michelle Bradshaw, DC, OTR/L for her assistance with this case report.
ABSTRACT
Occupational therapy with integrative health approaches in a community setting improved occupations for a woman with Bipolar and Anxiety Disorders. A 40-year-old woman with a history of Bipolar Type I and II and an Anxiety Disorder received occupational therapy sessions for six weeks to improve her occupations. Client reported decreased stress and anxiety levels, increased participation in activities of daily living, increased physical activity and exercise, and overall improved sleep quality. Occupational therapy with integrative health approaches may improve the ability for individuals with mental health conditions to increase participation and satisfaction in meaningful occupations.
KEYWORDS Mental health, bipolar, anxiety, integrative health, meditation
Introduction
This paper describes the effectiveness of occupational therapy (OT) with integrative health approaches in a community setting for a woman with Bipolar and Anxiety Disorders.
Mental health
Occupational therapy has its roots in mental health. Mental illness can significantly affect an individual’s ability to engage in meaningful activities of daily living and productive daily routines (AOTA, 2016). Mental disorders are among the most common causes of disability. In 2014, an estimated 18.1% (43.6 million) of U.S. adults ages 18 years or older have suffered from any mental illness and 4.1% (9.8 million) suffered from a seriously debilitating mental illness (Hedden, S. L., Copello, E. A. P., Kennet, J., Kroutil, L. A., Lipari, R., Medley, G., Tice, P., 2015).However, since 2009, the number of research articles on occupational therapy in the practice area of mental health published in the American Journal of Occupational Therapy (AJOT) is less than the number of research articles in all other practice areas except work and industry, and health and wellness (Gutman, S.A. & Raphael-Greenfield, E., 2014), suggesting the intervention focus for OT has shifted back to an earlier emphasis on prevention and wellness, using daily activities within a natural context in order to provide a holistic perspective for intervention (Burroughs, T., Mathieson, K., Belden, C.V., Gross, M., 2016).
There is a growing body of psychoneuroimmunological research linking physical health to emotional well-being (Lattie, E. G., Antoni, M. H., Fletcher, M. A., Penedo, F., Czaja, S., Lopez, C., … Klimas, N., 2012). The state of a person’s mental health can play a major role in their ability to maintain good physical health. Mental illnesses can affect people’s ability to participate in health-promoting behaviors. Challenges with physical health, such as chronic diseases, can have a serious influence on mental health and lower a person’s ability to participate in treatment and recovery (Lando, J., Marshall Williams, S., Sturgis, S., & Williams, B., 2006). Occupational therapy provides care for people with both physical and mental illness.
Integrative health, wellness and prevention
Health and Wellness is one of the six key OT practice areas, and possible outcomes from OT intervention (AOTA, 2014). The mainstream health care system in the United States has functioned primarily in the acute care or “sick care” biomedical model that addresses disease after a person has become ill and may be improved by providing a prevention model that focuses on health that forestalls disease development (Fani & Stafford, 2012). There is a call by Wendy Hildebrand, MPH, OTR/L, FAOTA and Amy Jo Lamb, OTD, OTR/L, FAOTA, president of the American Occupational Therapy Association, for occupational therapists to address health, wellness, and prevention (“Occupational Therapy in Prevention & Wellness”, 2013).
Integrative health care often combines conventional and complementary approaches together in a coordinated way. A holistic, patient-focused approach to health care and wellness is emphasized. It treats the whole person including the mental, emotional, functional, spiritual, social, and community aspects. When a non-mainstream practice is used together with conventional medicine, it’s considered “complementary.” When a non-mainstream practice is used in place of conventional medicine, it’s considered “alternative” (National Center for Complementary and Integrative Health, 2016).
According to the National Center for Complementary and Integrative Health (NCCIH), the use of an integrative approach for health and wellness has grown within care settings across the United States, including hospitals, hospices, and military health facilities since its inception 16 years ago (National Center for Complementary and Integrative Health, 2016).
The OT scope of practice may be supported by integrative health, when appropriate. OT has a similar holistic approach as integrative health. OT with integrative health may be used to improve clinical outcomes (AOTA, 2011).
Clinical case
Mary, a pseudonym, is a 40-year old educated Caucasian woman who lives with her husband and pets and has been sober from alcohol for 20 years. At age 30 she was diagnosed with Bipolar I after a psychotic episode and hospitalization. After two more hospitalizations, Mary’s diagnosis changed to Bipolar II at age 36. Additionally, Mary was diagnosed with an Anxiety Disorder and her symptoms of anxiety temporarily improved following a support group. Despite her use of clonazepam, as needed, for her symptoms of anxiety, Mary recognized that she was not fully engaging in her meaningful occupations and sought OT services.
Mary was seen by a mental health practitioner weekly and followed by a psychiatrist. She expressed interest in attending support groups, such as Alcoholics Anonymous or an anxiety group, that she has attended in the past, but reported feeling anxious about the required public speaking components of the groups. Mary denied any feelings of depression, but did express experiencing anxiety that can interfere with her ability to participate in meaningful occupations.
Occupational therapy assessments and findings
This case report was part of a Level 2 Fieldwork experience where the occupational therapy student (OTS) administered the initial OT assessments/evaluations under the supervision of the occupational therapist (OTR/L). Subsequent intervention sessions were co-led by the OTR/L and OTS to ensure proper administration of treatment methods. Mary was first seen for an initial evaluation that lasted 90 minutes followed by six visits averaging 90 minutes each.
Initial assessments
The Canadian Occupational Performance Measure (COPM) and the Kawa model were administered to Mary to determine her self-perception of overall occupational performance. The COPM is an outcome measure designed to be client-centered for occupational therapists to assess client outcomes in the areas of self-care, productivity and leisure (Law, Baptiste, McColl, Opzoomer, Polatajko, and Pollock, 1990). The Kawa model attempts to clarify the application of OT within the client’s particular social and cultural context. Kawa means river in Japanese and may have a symbolic meaning that provides a metaphor of a river being a person’s life where OT may help with a person’s life flow (Iwama, Thomson & Macdonald, 2009).
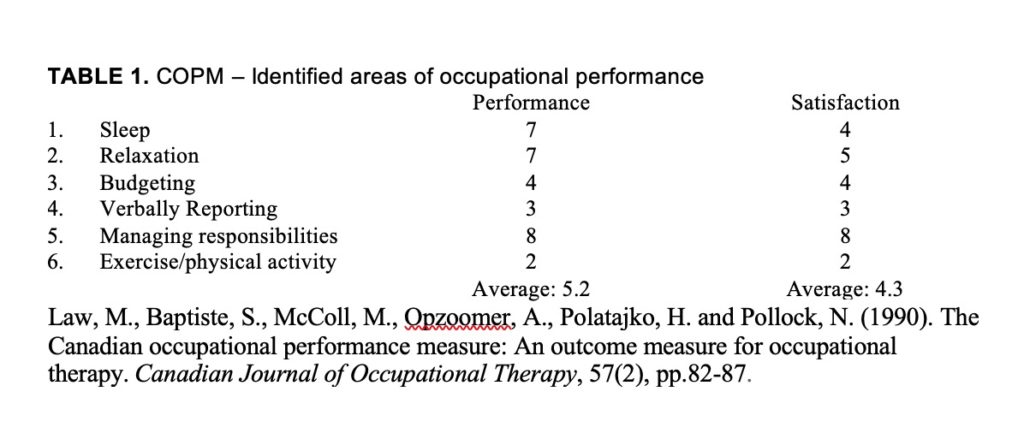
Based on the COPM’s semi-structured interview, Mary identified her top areas of occupational performance problem areas to be: Sleep, Relaxation, Budgeting, Verbally Reporting, and Managing Responsibilities. Anxiety seemed to be her primary client factor the impacted her successful participation in occupations (Table 1).
Kawa model was administered through an aerial view with paper and colored pencil and a cross section view on an iPhone app (Iwama, 2009 & Georgia Regents University, 2014). In the aerial view, Mary drew a river that appeared to be flowing well. However, when she completed the cross-section, Mary identified her obstacles and support were more spread out and that anxiety was her main obstacle. Her supports were work, friends, family, art and animals. She expressed that she would like her supports to be more connected and to surround her obstacles.
After completing the initial COPM (Table 1) and the Kawa Model Mary identified her top three occupational performance areas to address: sleep hygiene, stress management, and the ability to verbally report in a group.
Therapy goals:
The results of the assessments were discussed with Mary and long-term goals were established. By the fifth visit Mary had met her long-term goals 1 and 2 and the goals were reviewed. We updated her long-term goal 3 and created a new long-term goal 4 to reflect the changing needs of Mary.
Long term goal 1: By 6 weeks, client will be independent in sleep hygiene program as evidenced by report of staying asleep throughout the night.
Long term goal 2: Client will identify and implement three relaxation and coping strategies that will decrease reported anxiety to an average of 3/10 or less during activities of daily living (ADLs).
Long term goal 3: Client will be able to report verbally in a group at a decreased anxiety level of 5/10 or less.
New long term goal 3: By the 7th visit, client will be independent in diet and healthy meal planning.
New long term goal 4: By the 7th visit, client will participate in home exercise program at least 5 times per week to manage stress and anxiety, aid in weight management and prevent further illness and disease.
Strategies, interventions and outcomes
Multiple OT and integrative health strategies and interventions were used. Below are a summary of Mary’s sessions and illustrate her response to OT and integrative health services.
Visit 2:
Mary reported feeling stressed at 6/10 as she felt pressure to complete several errands prior to her OT session. An interventions strategy consisted of her creating a priority-based to-do list to help organize her days/week to reduce her feelings of stress with completing tasks. Anxiety and low self-esteem may be correlated (Mruk, 2013). Therefore, she completed the Sorenson Self-Esteem Test. She scored a 16/30 indicating moderately low self-esteem. We guided her in abdominal breathing, progressive relaxation, and a special imagery. We recommended that Mary meditate by practicing these techniques for five minutes, three times in the next week, as research has found that participating a relaxation techniques or activities and meditation can reduce stress and anxiety levels (Benson, H. & Proctor, W., 2010). We then educated her on sleep hygiene tips from the American Sleep Association, and recommended she try completing a reflection journal nightly to aid with falling asleep, as she had mentioned this was something she had done years ago and has improved her ability to fall asleep (The American Sleep Association, 2016). Her reported stress level decreased to a 2/10 at the end of the session.
Visit 3:
Mary rated her stress level at a 3/10. She stated, “The meditation I did today before coming in put me in a great mood. I am much more calm.” She reported that the relaxation techniques were “going great” for her. She identified a relaxation activity of making art. She also read a book, participated in a dance event, went for a walk, and a bike ride that were all relaxing for her. She did not complete the sleep journal as it was too cumbersome. Her cats were disturbing her ability to sleep as they would scratch her bedroom door and took up too much space in her bed. We recommended she look in to a cat scratching post or cat house to give them another space to go during the night. When discussing nightly routines, Mary identified that she used to reflect on her day every night before going to bed, and it would help her fall asleep. However, she hadn’t participated in reflection for a number of years stating, “I can’t remember why I stopped.” We recommended that she try to reflect before bed nightly for one week.
Mary reported her consumption of sugary drinks was more than she would like to admit, and she recognized that this might have been interfering with her energy, mood, and stress and anxiety levels. She identified Kombucha as a substitute she would like to use. Mary reported practicing eight minutes of meditation three times per week and found a few online meditations she really liked. We recommended that she increase her meditations to 10 minutes three times for the upcoming week. At the end of session Mary rated her stress at a 3/10 as well.
Visit 4
Mary stated “I am feeling good today.” Her stress was a 3/10. She reported that her priority-based to-do lists assisted her to complete more of her daily tasks. She also reported success with reading for leisure, reflection before bed, and weekly meditations.
However, she noted difficulty with substituting sugary drinks as after three days without drinking any, she drank seven in one day. On one day, she felt highly stressed and took four Seroquel and three Klonopin. The rest of the week she had less stress. She reported meditations were reducing her anxiety. The reading and meditations were starting to become more routine and that the reflection before bed had been helping her sleep. She had not woken up during the night. We educated Mary on reading food labels, healthy portion sizes, and pairing of healthy foods that supported her weight loss goals. We provided her with resources such as the “Australian Guide for Healthy Eating” and the Centers for Disease Control and Prevention (CDC), “Healthy Eating for healthy weight” (The Australian Guide to Healthy Eating, 2016, The Centers for Disease Control, 2016).
We also instructed her on how to perform mindfulness meditation to aid in identifying triggers associated with stressful situations and observe thoughts and feelings with less judgement and more compassion during her daily occupations.
Visit 5:
Mary reported completing errands prior to the session. She stated, “I probably shouldn’t have done so much.” Her stress level was at a 4/10. Mary completed a food intake journal. We encouraged her to identify foods she could include to make her meals more balanced and nutritious while using information from the CDC and Australian healthy meal planning guide.
Mary reported having met her long-term goals 1 and 2 related to sleep hygiene and relaxation. She expressed that her long-term goal of verbally reporting was not an area of priority for her at the time. Therefore, we changed short term goal 3 to address healthy meal planning, diet and exercise to new long-term goal 4.
Visit 6:
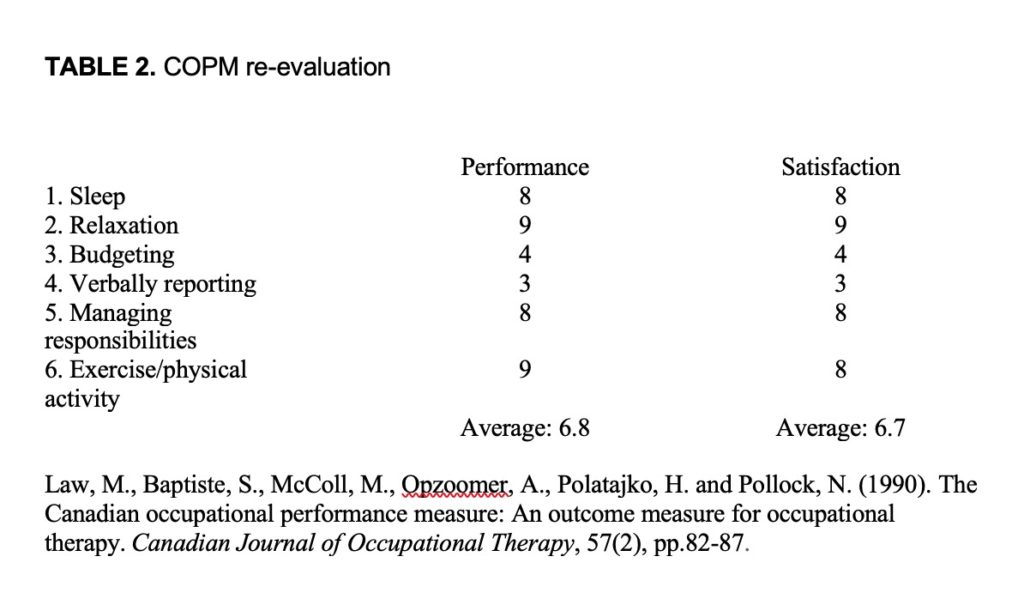
Client reported, “I’ve been doing a lot better with relaxing and sleeping since I started working with you.” We re-evaluated the COPM for sleep and relaxation. She was receptive to the meal planning and a home workout for beginner’s handouts were provided.
Visit 7:
Mary completed her exercises, but felt they were an effort to do. She reported walking three times in the past week, completed two 20-minute workout videos, including yoga. She also completed her home exercise hand-out three days during the week and stretched daily. She reported walking outside was too cold due to winter. We recommended walking at the mall, stores, taking stairs, and parking further away from stores. We suggested that she could combine meditation and stretching. She identified that moving was the best way to keep her active. We suggested that she find exercise and movement activities that she might enjoy, because then she will be more likely to engage in these activities. She had identified that she enjoyed dancing. We re-evaluated the COPM for occupational performance for healthy meal planning and physical activity.
We assessed how likely Mary thought she would continue with the approaches she received during the visits. Mary reported an 8/10 likelihood that she would continue with physical activity. She had removed all unhealthy snacks from her home and was using the suggested snack ideas from the healthy meal planning handouts. She stated that the likelihood for her to continue with healthy meal planning was a 10/10.
Mary reported being grateful for her experience with occupational therapy with integrative health. “I now feel like things I used to worry about don’t seem so bad. I worry less and I’m suppressing less. The meditations can make things that seem like a big deal not so bad and reflection helps keep me calm. Mindfulness helps me be less judgmental of things that have happened during the day and in the past. I have a greater appreciation for the things around me and my support system.”
Mary noted that her spirituality has increased over the seven sessions stating that it had become an unexpected improved area of occupation in her life. “Spirituality feels like a whole new world. The meditation is really great – you can feel peace about everything. I don’t have to worry so much. I feel so confident when I meditate. The reflection reminds me of my old self. I would be afraid to close my eyes. The thoughts… I would just want to be knocked out and go to sleep. It feels like I’m not judging myself and I’m better able to participate in the activities I enjoy.”
At the end of our visits, we recommended that Mary continue with occupational therapy to address verbally reporting in a group and/or to address this with her mental health practitioner.
Re-evaluation
We re-evaluated with the COPM (Table 2) at the sixth and seventh visits. Mary’s occupational performance average increased from 5.2/10 to 6.8/10 and her satisfaction increased from 4.3/10 to 6.7/10. Her occupational performance for sleep increased from 7/10 to 8/10 and her satisfaction increased from 4/10 to 8/10 from the initial evaluation. Her occupational performance for relaxation increased from 7/10 to 9/10 and her satisfaction increased from 5/10 to 9/10. Her occupational performance for healthy meal planning and physical activity increased from 2/10 to 9/10 and her satisfaction increased from 2/10 to 8/10 (Tables 1 and 2).
The KAWA Model was re-evaluated at the sixth session. Mary identified her obstacles and supports felt closer together which she explained as symbolizing unity and a sense of connection with each other that felt better to her. At the initial evaluation she identified that her obstacles and support were more spread out and expressed that she would like her supports to be more connected and to surround her obstacles at the initial evaluation.
She completed the Sorensen Self Esteem Test and scored indicating an improvement to mild self-esteem 7/30 from moderately low self-esteem 16/30.
Discussion
This case report attempts to demonstrate the effectiveness of OT with integrative health approaches in a community setting for a woman with Bipolar and Anxiety Disorders to engage in meaningful activities of daily living and productive daily routines.
Occupational performance and satisfaction increased in all identified areas of occupational performance for Mary. Overall, we were encouraged with the level of reported improvements Mary had with her daily occupational performance and decrease in anxiety symptoms within six sessions. We found the COPM and Kawa model can assist well with identifying occupational performance areas and assist with health, wellness, and prevention.
One of the limitations identified within this case study was the time frame in which therapy was provided. Mary was provided OT interventions for six visits. However, with a longer treatment period, we could have further supported her movement and fitness goals for greater adherence. The occupational performance goal of verbally reporting could have also been addressed as it was earlier identified as a priority for Mary.
Further research is needed to determine the optimal time frame in which therapies could be provided to clients to develop long term carryover.
Conclusion
This case study begins to highlight how occupational therapy with evidence-based integrative health approaches may improve the ability for clients with mental health diagnoses to engage in meaningful occupations.
Informed consent
The patient read this case report to confirm its content and gave verbal consent to publish.
References
American Occupational Therapy Association (AOTA). Giese, T. (2011). Complementary and
Alternative Medicine Position Paper. American Journal of Occupational Therapy, 65(Supplement_6), doi:10.5014/ajot.2011.65S26
American Occupational Therapy Association. (2014). Occupational Therapy Practice framework: Domain and process(3rd Ed.). American Journal of Occupational Therapy, 68(139). doi:10.5014/ajot.2014.682005
The American Occupational Therapy Association (2016). Occupational Therapy’s Role in Community Mental Health. Retrieved December 16, 2016, from htt://www.aota.org/about-occupational-therapy/professionals/mh/community-mental-health.aspx
The American Sleep Association (2016). Sleep Hygiene. Retrieved December 16, 2016, from American Sleep Association
Eatforhealth.gov.au. (2016). The Australian Guide to Healthy Eating. Retrieved December 16, 2016, from https://www.eatforhealth.gov.au/guidelines/australian-guide-healthy-eating
Benson, H. & Proctor, W. (2010). Relaxation Revolution: Enhancing Your Personal Health Through the Science and Genetics of Mind Body Healing. New York, NY: Simon and Schuster, Inc.
Burroughs, T., Mathieson, K., Belden, C.V., Gross, M. (2016). A Qualitative Study of the Role of Occupational Therapy in Mental Health Community-Based Settings. American Journal of Occupational Therapy, 70, 7011505136p1. doi:10.5014/ajot.2016.70S1-PO4031
Centers for Disease Control and Prevention. (2016). Health Eating for Healthy Weight. Retrieved December 16, 2016, from https://www.cdc.gov/healthyweight/healthy_eating/
Fani Marvasti, F., & Stafford, R. S. (2012). From sick care to health care–reengineering prevention into the U.S. system. The New England journal of medicine, 367(10), 889–891. doi:10.1056/NEJMp1206230
Georgia Regents University. (2014). Kawa (82.9 MB). [Mobile application software]. Retrieved December 16, 2016, from https://itunes.apple.com/us/app/kawa/id882899927?mt=8.
Gutman, S.A. & Raphael-Greenfield, E. (2014). Five Years of Mental Health Research in the American Journal of Occupational Therapy, 2009–2013. American Journal of Occupational Therapy, 68, e21-e36. doi:10.5014/ajot.2014.010249
Hedden, S. L., Copello, E. A. P., Kennet, J., Kroutil, L. A., Lipari, R., Medley, G., Tice, P., Center for Behavioral Health Statistics and Quality. (2015). Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health (HHS Publication No. SMA 15-4927, NSDUH Series H-50). Retrieved December 16, 2016, from http://www.samhsa.gov/data/
Hildenbrand. W. & Lamb, A. (2013). Occupational Therapy in Prevention & Wellness: Retaining Relevance in a New Health Care World. American Journal of Occupational Therapy, 67, 266-271. doi: http://ajot.aota.org/Article.aspx?articleid=1851676
Iwama, M. K., Thomson, N. A., & Macdonald, R. M. (2009). The Kawa model: The power of culturally responsive occupational therapy. Disability and Rehabilitation, 31, 1125-1135.
Lando, J., Marshall Williams, S., Sturgis, S., & Williams, B. (2006). A Logic Model for the Integration of Mental Health into Chronic Disease Prevention and Health Promotion. Preventing Chronic Disease, 3(2), A61.
Lattie, E. G., Antoni, M. H., Fletcher, M. A., Penedo, F., Czaja, S., Lopez, C., … Klimas, N. (2012). Stress management skills, neuroimmune processes and fatigue levels in persons with chronic fatigue syndrome. Brain, Behavior, and Immunity, 26(6), 849–858. http://doi.org/10.1016/j.bbi.2012.02.008
Law, M., Baptiste, S., McColl, M., Opzoomer, A., Polatajko, H. and Pollock, N. (1990). The Canadian Occupational Performance Measure: An Outcome Measure for Occupational Therapy. Canadian Journal of Occupational Therapy, 57(2), pp.82-87.
Mruk, C. (2013). Self-Esteem and Positive Psychology, 4th Edition: Research, Theory, and Practice. New York, NY: Springer Publishing Company
National Center for Complementary and Integrative Health (2016). Complementary, Alternative, or Integrative Health: What’s in a Name? Retrieved December 16, 2016, from https://nccih.nih.gov/health/integrative-health